Intraocular medical devices development encompasses the design, testing, and regulatory validation of implantable technologies for treating severe ocular conditions. The global ophthalmic devices market reached $46.14 billion in 2024, with projections indicating growth to $73.74 billion by 2034 at a compound annual growth rate of 4.80%. North America captured 43% of revenue share, driven by rapid adoption of advanced intraocular lenses and high volumes of cataract surgeries.
Recent clinical data demonstrate tangible outcomes. The intraocular lens market valued at $4.27 billion in 2024 is projected to reach $7.36 billion by 2034, reflecting increased demand for premium lenses. Biotechfarm provides specialized pre-regulatory large animal studies and Good Laboratory Practice validation essential for advancing these technologies from concept to clinical application.
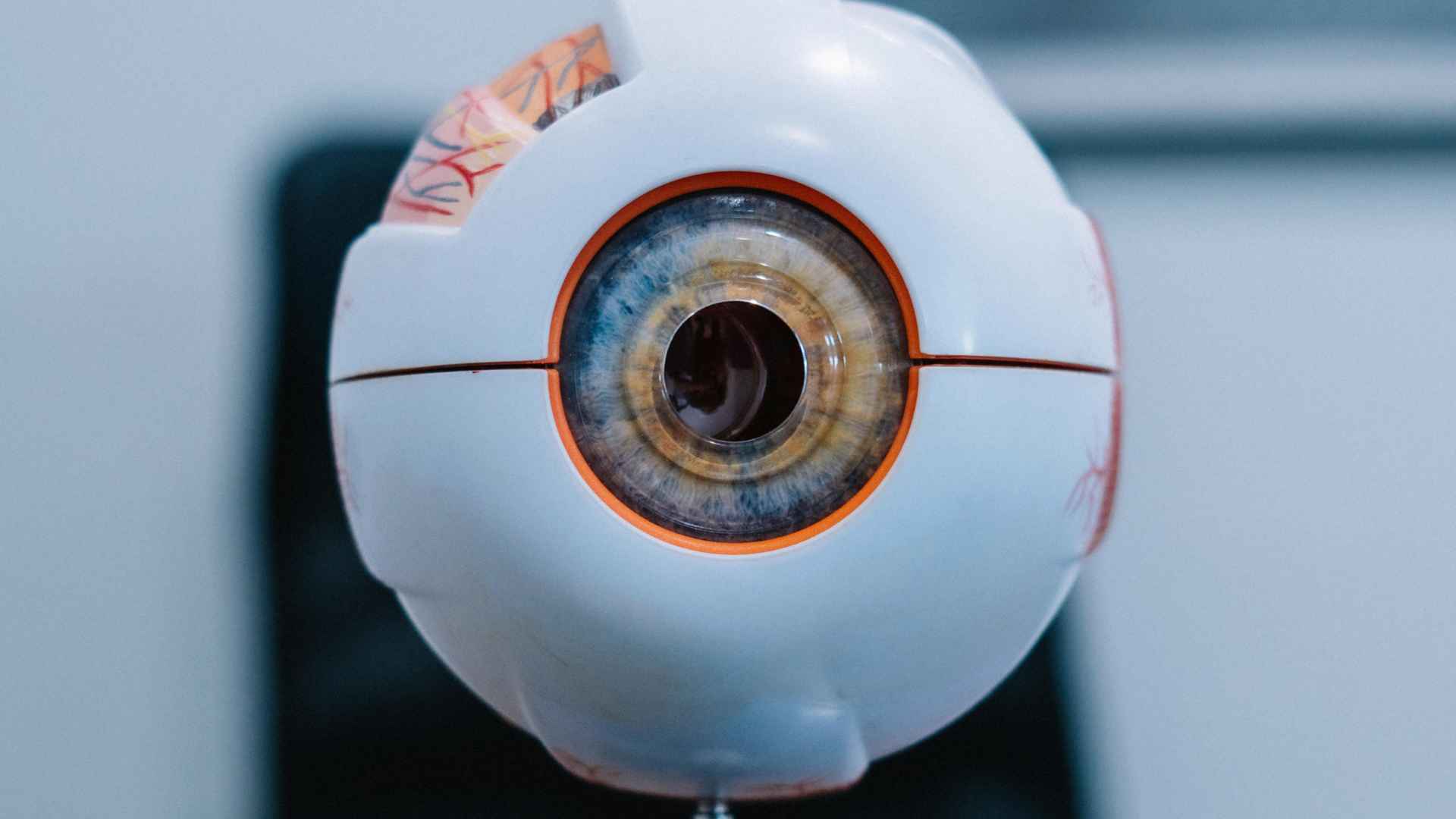
What Are Intraocular Medical Devices and Their Primary Applications?
Intraocular medical devices are surgically implanted technologies that restore or enhance eye function. The main applications fall into three categories: optical correction devices like intraocular lenses (IOLs) used primarily after cataract surgery, which represented 85-90% of market revenue in 2024; sustained-release drug delivery implants for treating glaucoma and retinal diseases; and retinal prostheses that stimulate neural tissue in patients with photoreceptor loss.
IOLs include monofocal, multifocal, and toric variants, with hydrophobic acrylic materials dominating 65-70% of the market due to better biocompatibility. Each device category requires specific development protocols: IOLs undergo standardized regulatory testing, drug implants need pharmacokinetic validation, and neural devices require bioelectrical compatibility assessments. Biotechfarm evaluates these technologies using large animal models that closely approximate human eye anatomy and physiology.
Clinical Validation Methodologies in Intraocular Medical Devices Development
Intraocular device validation follows ISO 10993 biocompatibility standards, evaluating cytotoxicity, sensitization, and irritation. Material selection critically influences outcomes hydrophobic acrylic lenses consistently outperform polymethyl methacrylate designs in clinical endpoints.
Large animal models provide anatomically relevant surgical platforms. Canine studies of latanoprost implants demonstrated sustained intraocular pressure reduction over 34 weeks without inflammatory responses, establishing dosing parameters for human trials.
FDA approval requires comprehensive Good Laboratory Practice evidence. The travoprost intracameral implant achieved clearance after phase 3 trials showed 81% medication-free rates at 12 months with 24-30% mean pressure reduction validating the preclinical-to-clinical pathway.
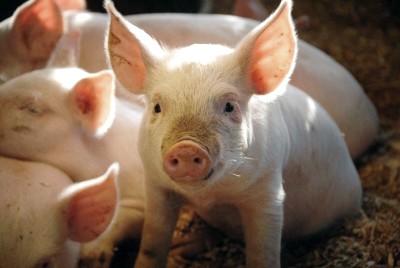
Species selection impacts study validity. Rabbit eyes serve initial toxicity screening despite thinner corneas and larger vitreous cavities. Non-human primates offer superior anatomical correlation but face ethical constraints. Porcine models balance practicality with comparable axial length and trabecular meshwork structure for glaucoma device assessment.
What Sustained-Release Drug Delivery Technologies Are Currently in Development for Glaucoma Treatment?
Sustained-release implants tackle a critical problem: poor medication adherence. Studies show patients miss topical eye drop doses 20-50% of the time, significantly reducing treatment effectiveness.
FDA-approved options include the bimatoprost implant (Durysta, 2020) lasting 4-12 months, and the travoprost implant (iDose TR, 2024) delivering medication for 2 years. Both demonstrated sustained IOP reduction in Phase 3 trials.
Emerging technologies push boundaries further. The SpyGlass platform integrates bimatoprost into intraocular lenses during cataract surgery, showing 43.7% IOP reduction over 18 months with potential 3-year duration. Contact lens systems like LL-BMT1 achieved 5.5 mm Hg pressure reduction in Phase 2b trials.
Biodegradable implants, such as the Latanoprost FA SR, dissolve within 4-6 weeks after delivering medication, eliminating surgical removal while maintaining efficacy through periodic re-implantation.
Retinal Prosthesis Technologies: Current State and Clinical Outcomes
Retinal prostheses restore partial vision in patients with photoreceptor loss while maintaining intact posterior visual pathways. The global retinal implants market reached $54.10 million in 2024, projected to expand to $122.32 million by 2034 at 8.50% CAGR, with North America commanding 37.5% market share.
The PRIMA subretinal implant demonstrated breakthrough outcomes in October 2024. Among 38 participants with advanced geographic atrophy, 27 regained reading ability after one year, with average improvement of 4.6 lines on standard eye charts some gaining nearly 12 lines. Participants recognized playing cards and completed crossword puzzles, with the photovoltaic chip operating wirelessly.
Device architecture determines performance. Epiretinal devices like the FDA-approved Argus II stimulate ganglion cells directly through 60-electrode arrays. Subretinal implants stimulate bipolar cells, exploiting residual retinal processing. Emerging suprachoroidal devices offer less invasive implantation between sclera and choroid, presenting reduced surgical risk despite lower resolution.
What Are the Primary Technical Challenges in Intraocular Medical Devices Development?
Developing intraocular devices faces three critical obstacles. Biocompatibility demands materials that resist protein buildup and inflammation while maintaining optical clarity for decades. Hydrophobic acrylic materials outperform earlier formulations, though glistening and posterior capsule opacification remain concerns.
Surgical constraints pose significant limitations. Standard cataract incisions measuring 2.2-2.8mm require foldable designs for IOLs, while drug delivery implants must navigate gauge-specific needles without compromising sterility. The travoprost implant uses specialized injectors for precise angle placement.
Power delivery challenges affect electronic devices. Early retinal prostheses needed transcutaneous cables, limiting mobility. Modern systems use wireless inductive coupling, but power efficiency restricts stimulation capacity. The PRIMA implant converts infrared light directly to electrical current, eliminating external power requirements entirely.
Material degradation impacts device longevity. PLGA microspheres undergo hydrolytic breakdown, with release rates dependent on polymer composition. Achieving predictable drug elution over months requires rigorous formulation control and accelerated aging protocols to ensure long-term stability.
How Do Preclinical Large Animal Studies Advance Intraocular Medical Devices Development?
Large animal models provide critical evaluation platforms before human trials. Species selection depends on device type porcine and canine models offer eye dimensions approximating human proportions while maintaining practical feasibility.
Glaucoma device development utilizes established canine models. Beagles with laser-induced ocular hypertension enable controlled evaluation of pressure-lowering interventions. The ENV515 travoprost implant study demonstrated sustained IOP reduction over 11 months with minimal adverse effects, informing phase 2 human trial parameters.
Specialized facilities conduct pre-regulatory studies under Good Laboratory Practice standards. Longitudinal monitoring protocols assess surgical healing, device stability, and tissue response through advanced imaging like optical coherence tomography. Histopathological analysis provides definitive biocompatibility evidence.
Regulatory agencies require specific endpoints: IOLs need refractive predictability within 0.50 diopters; drug delivery devices must demonstrate sustained therapeutic levels; retinal prostheses require neural stimulation evidence without tissue damage.
What Role Does Biotech Farm LTD Play in Advancing Intraocular Medical Devices Development?
Biotech Farm operates a specialized large animal research facility advancing ophthalmic device technologies through comprehensive preclinical testing services. Founded by Adir Koreh and Rinat Borenshtain-Koreh, professionals with over 30 years of research leadership, the facility supports companies from concept validation through regulatory submission.
Core capabilities include pre-regulatory safety studies, complex intraocular surgical expertise (vitrectomy, retinal repair, implant positioning), and GLP-compliant safety studies generating FDA-required documentation. The collaborative model emphasizes close communication with developers, iterative protocol modifications, and post-study consultations for regulatory planning.
Testing spans intraocular lens evaluation, drug delivery system pharmacokinetics, and electronic implant assessments. Rigorous ethical standards, veterinary oversight, and transparent reporting practices deliver comprehensive data packages supporting regulatory submissions. This positions Biotech Farm as a trusted partner in the competitive intraocular medical devices landscape.
How is Biotech Farm Positioned to Support the Next Generation of Intraocular Medical Devices Development?
Biotech Farm addresses the evolving demands of intraocular device validation through strategic infrastructure investment and technical expertise. The facility supports emerging technologies including gene therapy vectors, optogenetic systems, and nanoparticle delivery platforms that require sophisticated preclinical assessment.
Advanced imaging capabilities provide the foundation for characterizing next-generation devices. Optical coherence tomography angiography enables non-invasive visualization of retinal vasculature and drug distribution patterns. Electroretinography delivers objective functional assessments following therapeutic intervention. These modalities generate the regulatory-grade data required for submission packages.
The team brings cross-platform experience spanning artificial corneas, trabecular meshwork stents, and intravitreal delivery systems. This breadth informs study design and enables rapid troubleshooting when unexpected findings arise. Biotech Farm partners with innovators developing breakthrough vision restoration technologies, providing the scientific rigor needed to advance transformative therapies from concept to clinical application.
FAQ
What regulatory requirements govern intraocular medical devices development?
Intraocular devices fall under Class II or Class III medical device classifications depending on risk profile. Class III devices, including retinal prostheses and some drug delivery systems, require Premarket Approval demonstrating reasonable assurance of safety and effectiveness through clinical trials. Class II devices, such as many intraocular lenses, qualify for 510(k) clearance by demonstrating substantial equivalence to predicate devices. Both pathways require biocompatibility testing per ISO 10993 standards, manufacturing quality system compliance under ISO 13485, and comprehensive risk analysis documentation. International markets impose additional requirements including CE marking in Europe and PMDA approval in Japan.
How long does intraocular medical devices development typically require from concept to market approval?
Development timelines vary significantly by device complexity and regulatory pathway. Simple intraocular lenses leveraging existing materials may achieve 510(k) clearance within 3-5 years from initial concept. Novel drug delivery systems typically require 5-7 years including formulation optimization, preclinical studies, and phased clinical trials. Complex electronic devices like retinal prostheses often exceed 10 years due to technical challenges, extensive safety testing requirements, and prolonged clinical evaluation periods. The PRIMA retinal implant, for example, progressed from initial human implantation in 2002 to preliminary pivotal trial results in 2024, representing over two decades of development.
What success rates characterize intraocular medical devices development programs?
Success rates correlate with device novelty and technical complexity. Incremental improvements to established device classes, such as modified intraocular lens designs, demonstrate relatively high approval rates exceeding 70%. Novel mechanisms face greater uncertainty, with estimates suggesting 30-40% of early-stage programs ultimately achieve regulatory approval. Attrition occurs primarily during preclinical phases when biocompatibility or performance issues emerge, and during clinical trials when safety concerns or insufficient efficacy become apparent. Adequate preclinical characterization through rigorous large animal studies significantly improves subsequent clinical success probability by identifying and addressing potential issues before human exposure.
What are the primary cost drivers in intraocular medical devices development?
Development costs accumulate across multiple phases. Material development and device fabrication constitute initial expenses, typically ranging from hundreds of thousands to millions of dollars depending on complexity. Preclinical studies including biocompatibility testing and large animal evaluations add substantial costs, with comprehensive GLP-compliant programs exceeding $500,000. Clinical trials represent the largest expense, with phase 3 programs for Class III devices potentially costing $20-50 million. Manufacturing scale-up, quality system establishment, and regulatory submission preparation add additional millions. Total development costs for complex Class III devices commonly exceed $100 million from concept through approval.
The Role of AI in biotech Farm’s Intraocular Medical Device Innovation
Artificial intelligence enhances multiple development aspects in intraocular medical devices. In retinal prostheses, AI algorithms optimize visual signal processing, improving pattern recognition and spatial orientation beyond simple electrode stimulation. Machine learning models predict optimal stimulation parameters based on individual patient anatomy and disease characteristics. Biotech Farm’s research sponsors leverage these AI capabilities during development to accelerate design optimization by modelling thousands of parameter combinations in silico before physical prototyping. Image analysis algorithms automate assessment of device safety and performance in preclinical studies, reducing analysis time and improving consistency. These applications are driving next-generation device capabilities and streamlining development timelines, positioning biotech Farm at the forefront of AI-integrated medical device innovation.
For companies developing intraocular medical devices and seeking to integrate cutting-edge AI capabilities into their development processes, biotech Farm offers specialized expertise and proven methodologies. Contact biotech Farm LTD today to explore how AI-driven innovation can accelerate your device development timeline and enhance clinical outcomes.